ADVERTISEMENT
Many women over 40 notice changes in their menstrual cycles, energy levels, or pelvic area that feel off but seem too minor to mention. These shifts often get brushed aside as “just part of aging” or stress, yet they can point to common uterine or hormonal concerns like fibroids, polyps, endometriosis, or perimenopause transitions. Ignoring them sometimes allows discomfort to build quietly over time. The good news is that paying attention early and talking with a healthcare provider can make a real difference in managing your well-being.
In this guide, we’ll explore 12 potential signals your body might be giving about uterine health. Stick around until the end – there’s a simple daily habit that many women find helpful for staying in tune with their bodies.

Why Uterine Health Matters After 40
As estrogen levels fluctuate during perimenopause, the uterus and surrounding tissues can respond in noticeable ways. Studies show that up to 70-80% of women experience uterine fibroids at some point, and many deal with abnormal bleeding or pelvic pressure during this stage of life. These changes aren’t always serious, but recognizing patterns helps you decide when to seek guidance.
Common conditions include:
- Uterine fibroids – noncancerous growths that can cause heavy periods or pressure.
- Endometrial polyps – small growths in the uterine lining linked to irregular bleeding.
- Endometriosis – tissue similar to the uterine lining growing outside the uterus, often causing pain.
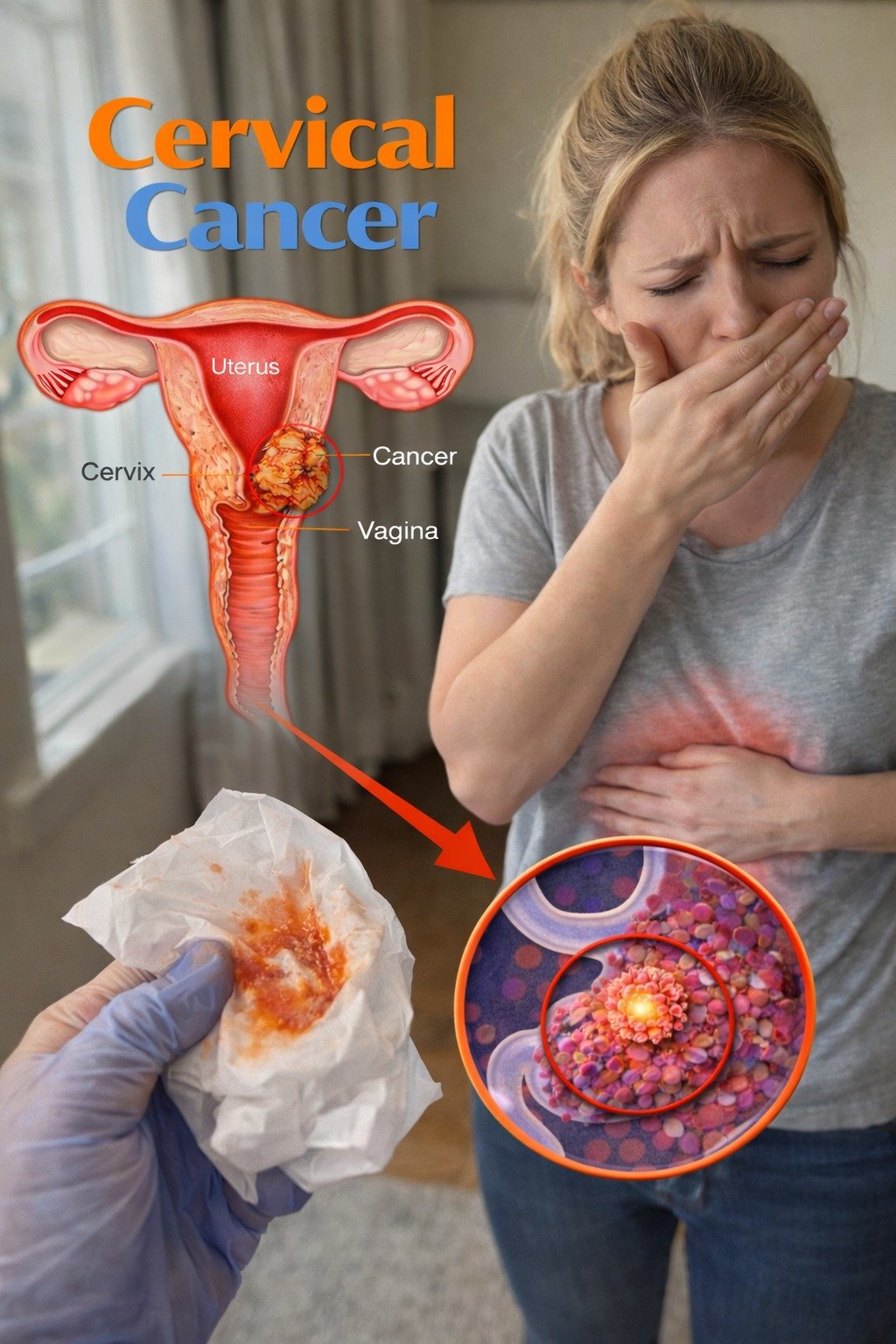
- Hormonal shifts that affect cycle regularity and energy.
Knowing what to watch for empowers you to take proactive steps.
1. Irregular or Unpredictable Periods
Your cycle suddenly becomes harder to predict – some months early, others late, or varying in length. This is one of the most reported changes after 40. Research in women’s health journals notes that irregular periods often tie to hormonal fluctuations or underlying uterine conditions.
Track your cycle for a few months using a simple app or calendar. Note the start date, flow, and any unusual timing.
2. Heavier-Than-Usual Menstrual Bleeding
Needing to change pads or tampons every hour or two, or passing large clots, can leave you feeling drained. Heavy bleeding is frequently associated with fibroids or polyps, according to studies in obstetrics and gynecology.
If this persists, it may lead to low iron levels over time. Consider monitoring how many products you use per day to discuss with your doctor.
3. Severe Menstrual Cramps That Disrupt Daily Life
Cramps that force you to cancel plans or rely heavily on pain relief aren’t typical “normal” discomfort. Severe pain can link to conditions like endometriosis or adenomyosis.
Heat packs, gentle stretching, or over-the-counter options may help short-term, but ongoing intensity deserves professional attention.

4. Pelvic Pain or Pressure Outside Your Period
A dull ache, heaviness, or sharp twinges in the lower abdomen or pelvis – even when not menstruating – can signal pressure from growths or other issues.
Many describe it as feeling like “something is sitting there.” Rate the discomfort on a scale to track changes over weeks.
5. Persistent Bloating or Abdominal Fullness
Feeling swollen or bloated most days, sometimes looking visibly distended, is common with uterine-related concerns. Unlike regular digestive bloating, this often doesn’t improve much with diet tweaks alone.
Stay hydrated and note if certain foods worsen it, but don’t dismiss it if it lingers.
6. Pain During or After Intimacy
Discomfort or pain during intercourse (known as dyspareunia) can affect closeness and confidence. This symptom appears in discussions of endometriosis, fibroids, or pelvic floor tension.
Open communication with a partner and gentle positions sometimes ease it temporarily, but addressing the root helps long-term.
7. Ongoing Fatigue That Doesn’t Improve with Rest
Feeling wiped out despite decent sleep is frustrating. Hormonal imbalances tied to uterine health can contribute to this persistent tiredness.
Prioritize consistent sleep hygiene, balanced meals, and light movement – but if fatigue dominates, it’s worth checking.
8. Needing to Urinate More Frequently or Urgently
Constant trips to the bathroom or a sudden strong urge, especially if paired with pelvic pressure, may relate to fibroids pressing on the bladder.
Track fluid intake and bathroom visits for a few days to spot patterns.
9. Changes in Vaginal Discharge
Unusual color, odor, consistency, or increased amount can indicate irritation or infection. Watery, bloody, or foul-smelling discharge warrants prompt attention.
Note any accompanying itching or irritation.
10. Lower Back Pain That Feels Connected to the Pelvis
Achy or constant lower back discomfort without clear injury can stem from uterine pressure or referred pain.
Gentle yoga poses or supportive seating may offer relief, but ongoing issues need evaluation.

11. Unexplained Weight Changes Around the Midsection
Sudden shifts in weight or difficulty managing it despite steady habits sometimes tie to hormonal fluctuations.
Focus on nutrient-dense foods and regular activity as supportive steps.
12. Increased Mood Swings or Emotional Sensitivity
Hormonal ups and downs can amplify irritability or tearfulness. While common in perimenopause, extreme shifts paired with physical symptoms deserve note.
Journaling moods alongside cycle tracking often reveals connections.
Practical Steps You Can Take Today
Here are a few low-effort habits to stay connected to your body:
- Daily tracking — Use a phone app or notebook to log periods, pain levels, energy, and other symptoms for 2-3 months.
- Pelvic check-ins — Once a week, rate pelvic comfort on a 1-10 scale and note triggers.
- Lifestyle supports — Stay active with walking or yoga, eat iron-rich foods if bleeding is heavy, and manage stress with deep breathing.
- When to reach out — See a healthcare provider if any sign persists more than a few cycles, worsens, or affects daily life. Regular check-ups, including Pap tests and pelvic exams, remain key for early awareness.
These small actions help you spot trends early and feel more in control.
Conclusion: Tuning In Makes a Difference
Your body often sends gentle signals before things become more disruptive. By noticing changes like irregular bleeding, pelvic discomfort, or fatigue, you give yourself the chance to address them thoughtfully. Many women find relief and reassurance simply by starting the conversation with a trusted doctor.
Frequently Asked Questions
What is the most common uterine health concern after 40?
Heavy or irregular bleeding tops the list, often linked to fibroids, polyps, or perimenopause changes, based on women’s health research.
How do I know if my symptoms are “normal” aging or something else?
If symptoms interfere with work, sleep, intimacy, or energy for more than a few months, or if bleeding becomes very heavy or unexpected, it’s wise to get checked.
Can lifestyle changes help with uterine discomfort?
Yes – regular movement, balanced nutrition, stress reduction, and good sleep support overall pelvic health, though they don’t replace medical guidance when needed.
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any health concerns.
ADVERTISEMENT