ADVERTISEMENT
Osteoporosis in Menopause: Why Your Mom’s Back Is Hurting and What You Can Do
You go home for Christmas and notice your mom is standing a little more hunched than before. She rubs her lower back, moves more slowly, and complains about pain that “just won’t go away.” It’s easy to blame age or fatigue—but there may be something more going on.
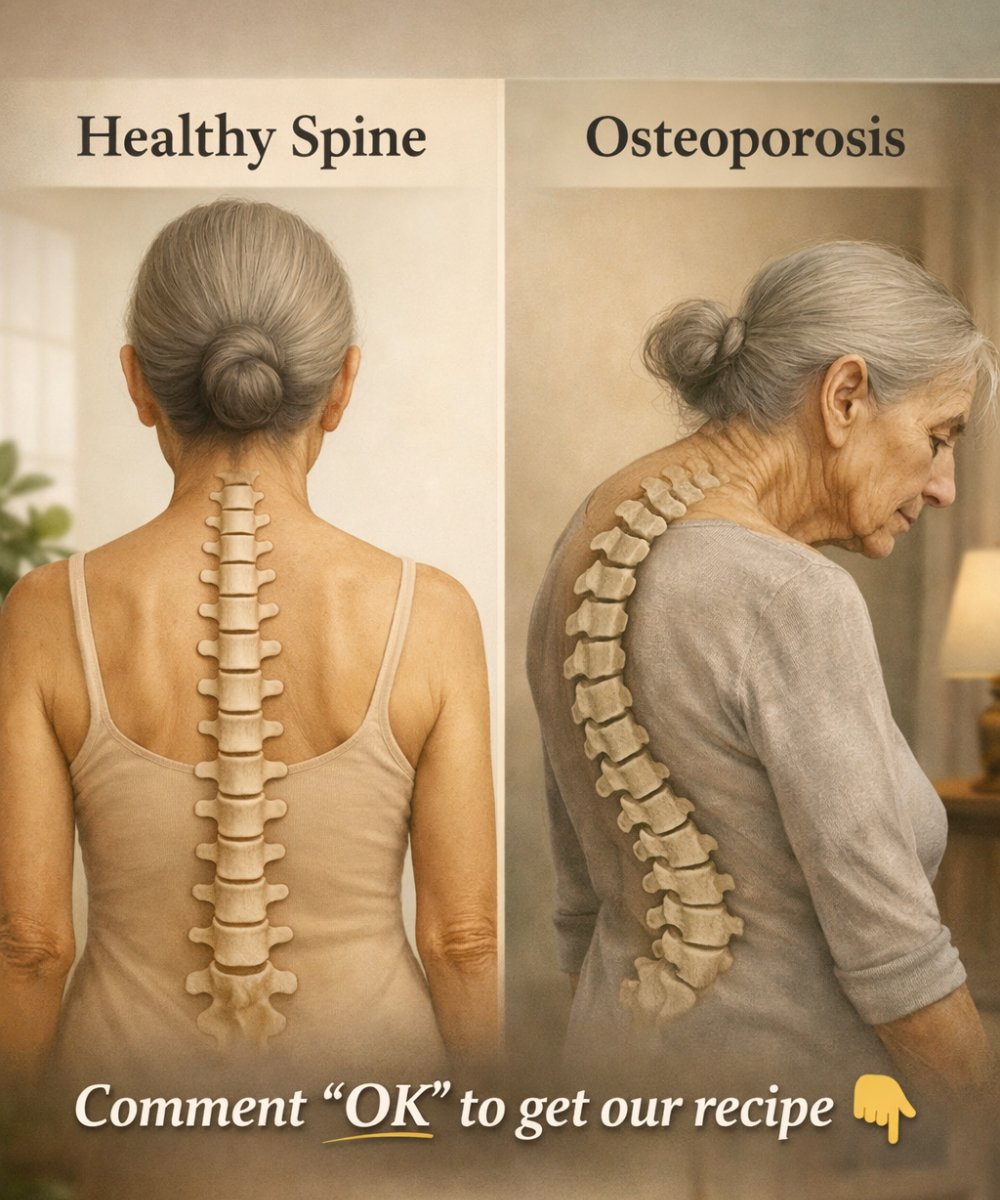
One common and often silent cause is osteoporosis in menopause. This condition weakens bones, changes posture, and increases the risk of fractures, especially in the spine. Understanding it early can make a real difference in comfort, mobility, and quality of life.
What Is Osteoporosis?
Osteoporosis is a condition where bones become less dense and more fragile. Healthy bones are strong and slightly flexible. With osteoporosis, bones lose minerals (especially calcium), become porous, and break more easily—even from minor falls or everyday movements.
The spine, hips, and wrists are the most commonly affected areas. In many women, the first signs show up in the back: chronic pain, loss of height, or a stooped posture.
Why Menopause Increases the Risk
Estrogen plays a key role in protecting bone strength. During menopause, estrogen levels drop sharply, and bone loss speeds up. In fact, women can lose a significant amount of bone density in the first 5–10 years after menopause.
This is why osteoporosis is much more common in postmenopausal women. Over time, small fractures in the spine (called compression fractures) can cause:
-
A hunched or stooped posture
-
Chronic back pain
-
Loss of height
-
Reduced mobility and balance
These changes often happen gradually, so families may not notice them until pain or posture changes become obvious.
Signs and Symptoms to Watch For
Osteoporosis is often called a “silent disease” because bone loss happens without pain at first. But as it progresses, symptoms may include:
-
Persistent or recurring back pain
-
A stooped or hunched posture
-
Getting shorter over time
-
Bones that break more easily than expected
If your mom is experiencing these signs, especially after menopause, it’s worth taking them seriously.
How Osteoporosis Causes Back Pain
In many cases, back pain comes from tiny fractures in the vertebrae (the bones of the spine). These fractures can happen from simple activities like bending, lifting light objects, or even coughing.
When several vertebrae weaken or collapse slightly, the spine can start to curve forward, leading to the classic hunched posture and ongoing muscle strain. This combination of bone changes and muscle fatigue is a common reason why back pain becomes chronic.
How to Ease Her Pain and Protect Her Bones
The good news: while osteoporosis can’t be “cured,” it can be managed. With the right steps, pain can be reduced and further bone loss can be slowed.
1. Encourage a Medical Check-Up
A doctor can assess bone health using a bone density scan (DEXA scan) and recommend appropriate treatment. This may include:
-
Calcium and vitamin D supplements
-
Medications that slow bone loss or strengthen bones
-
Pain management strategies for the back
Early diagnosis makes a huge difference.
2. Improve Daily Nutrition
Diet plays a big role in bone health. Focus on foods rich in:
-
Calcium: milk, yogurt, cheese, leafy greens, almonds, tofu
-
Vitamin D: fatty fish, eggs, fortified foods, and safe sun exposure
-
Protein: supports muscle strength and balance
Good nutrition helps support both bones and muscles, which can reduce pain and improve posture.
3. Gentle, Regular Exercise
The right kind of movement can actually strengthen bones and reduce pain. Helpful activities include:
-
Walking or light weight-bearing exercises
-
Strength training with light resistance
-
Balance and posture exercises
-
Stretching and gentle mobility work
Exercise helps improve posture, reduce stiffness, and lower the risk of falls. It’s best to follow a plan recommended by a doctor or physical therapist, especially if pain is already present.
4. Support Better Posture
Simple changes can reduce strain on the spine:
-
Use chairs with good back support
-
Avoid long periods of slouching
-
Keep screens and books at eye level
-
Consider posture-support exercises or physiotherapy
Better posture doesn’t just look better—it can significantly reduce back pain.
5. Make the Home Safer
Since osteoporosis increases fracture risk, preventing falls is crucial:
-
Remove loose rugs or clutter
-
Ensure good lighting
-
Add handrails in bathrooms or on stairs
-
Encourage supportive, non-slip footwear
Small changes at home can prevent serious injuries.
Emotional Support Matters Too
Chronic pain and posture changes can affect confidence and mood. Your mom might feel frustrated, older than she feels inside, or worried about losing independence. A little patience, encouragement, and support go a long way.
Sometimes, just knowing that the pain has a real, manageable cause can be a huge relief.
The Takeaway
If your mom seems more hunched and complains of back pain, it might not be “just age.” Osteoporosis in menopause is common, serious, and often overlooked—but it’s also manageable.
With early diagnosis, the right nutrition, gentle exercise, and proper care, it’s possible to reduce pain, protect her bones, and improve her quality of life. Paying attention now could help her stay stronger, more comfortable, and more independent for years to come.
ADVERTISEMENT