ADVERTISEMENT
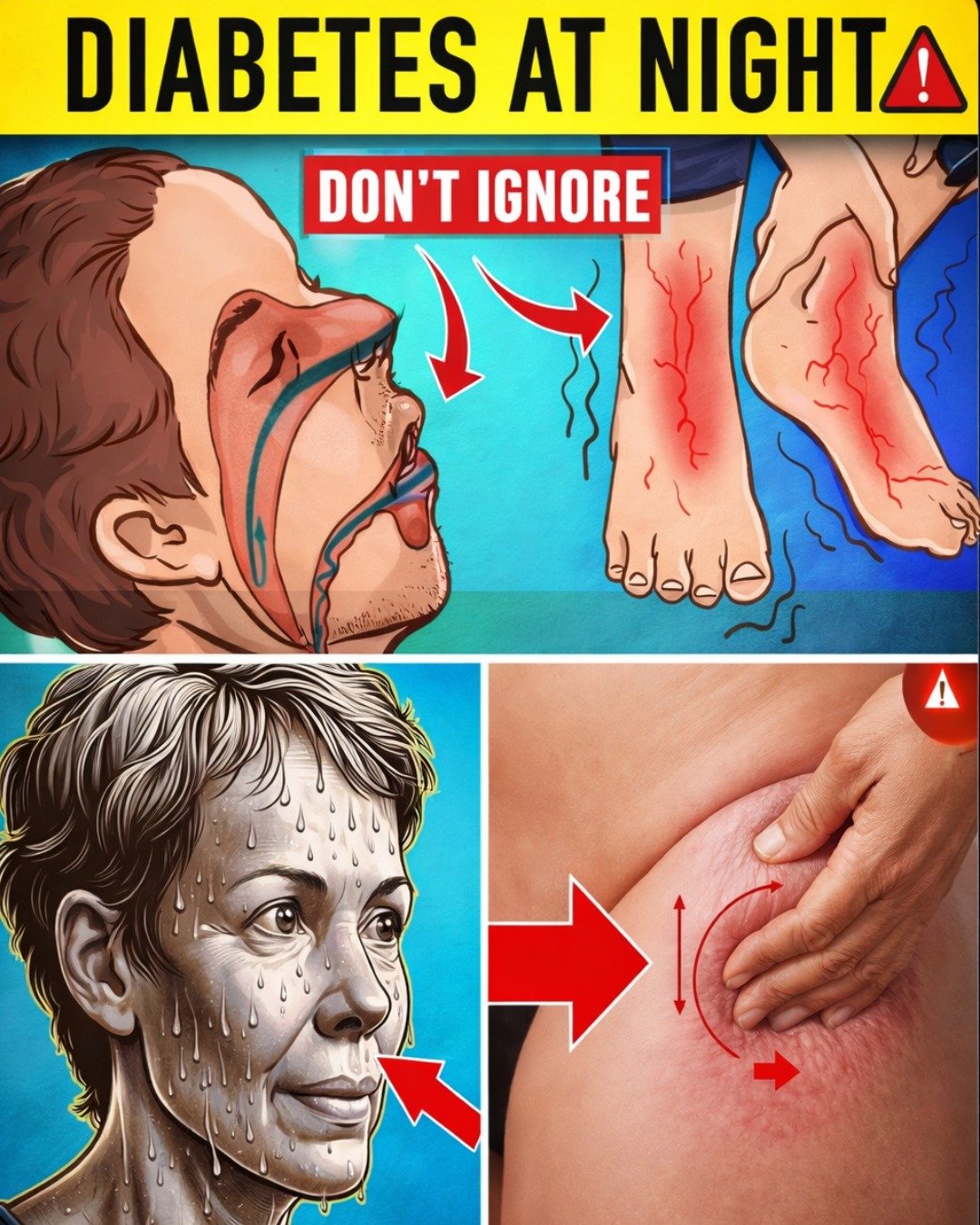
Over 38 million Americans live with diabetes, and about 8.7 million don’t even know they have it. Many of these undiagnosed cases show up first through subtle symptoms that strike at night, when blood sugar levels can swing wildly without you noticing. These disruptions steal your rest, leave you exhausted the next day, and quietly raise risks for serious complications.
It’s frustrating—tossing and turning, waking up multiple times, or feeling drenched in sweat for no clear reason. You might blame stress, aging, or a bad mattress. But what if these interruptions are your body’s urgent signals of unbalanced blood sugar? Ignoring them can worsen insulin resistance and lead to bigger health issues down the line.
The good news? Spotting these patterns early gives you a real chance to take control. Stick with me as we break down the 7 key nighttime signs, backed by science—and discover a simple plan that could help you wake up feeling truly refreshed.
Why Nighttime Symptoms Are a Big Deal for Blood Sugar Control
Diabetes doesn’t stop at bedtime. In fact, blood sugar fluctuations can be more unpredictable overnight when you’re not eating or moving around.
Research shows that poor sleep quality in people with diabetes can worsen insulin resistance, raise average blood sugar levels (like your A1C), and increase risks for heart problems. One cycle feeds the other: unstable glucose disrupts sleep, and lack of rest makes it harder for your body to manage blood sugar the next day.
Sound relatable? If you’re waking up more than once a night or feeling drained no matter how early you hit the pillow, it might not just be “normal” fatigue.
But here’s the encouraging part—many people regain deep, restorative sleep once they address these underlying imbalances. Let’s dive into the signs.
1. Night Sweats: Your Body’s Alarm for Low Blood Sugar
Waking up soaked in sweat, even in a cool room? This is one of the most overlooked nighttime clues.
It often happens due to nocturnal hypoglycemia—when blood sugar drops too low overnight. Your body releases stress hormones like adrenaline to raise glucose quickly, triggering profuse sweating.
Studies link these episodes to added strain on the heart. In real life, many people notice the sweats stop after small adjustments, like checking levels before bed.
What you can do right away:
- Test your blood sugar at bedtime.
- Keep a fast-acting carbohydrate (like glucose tabs) on your nightstand.
If this happens a few times a week, it’s worth discussing with your doctor.
2. Frequent Nighttime Urination (Nocturia): The Top Red Flag
Waking up two or more times to use the bathroom? This is often the most common—and dangerous—nighttime sign of high blood sugar.
When glucose levels are elevated, your kidneys work overtime to filter it out, pulling extra fluid into urine. The result: constant trips that fragment your sleep.
Science notes this as a classic indicator of uncontrolled diabetes, and it can signal ongoing high levels that raise complication risks.
One patient shared how reducing nighttime trips from 4–5 to just once transformed her energy. “I finally feel rested,” she said.
Quick tips to try:
- Limit fluids after 7 PM.
- Monitor daytime blood sugar for better overnight control.
- Track how many trips you make—more than two is a signal to pay attention.
You’re already ahead by reading this far. Keep going!
3. Restless Legs Syndrome: That Uncontrollable Urge to Move
Legs twitching or crawling sensations that keep you from settling down? This could tie back to nerve changes from prolonged high blood sugar.
Peripheral neuropathy—nerve damage—can cause tingling and irresistible urges to move your legs, worsening at night.
Research connects restless legs to diabetes, especially when glucose isn’t steady.
Practical steps:
- Aim for consistent blood sugar through the day.
- Try gentle evening stretches or a warm bath.
- Avoid caffeine after lunch.
Many find relief with these simple habits.
4. Nocturnal Hypoglycemia: The Silent Overnight Drop
This hidden low can strike without warning, leading to confusion, nightmares, or even more serious issues if untreated.
It’s especially risky because you’re asleep and might not wake up to treat it.
Continuous glucose monitors (CGMs) have been a game-changer for many, sending alerts before levels crash.
Safety strategies:
- If bedtime readings are borderline, have a small protein-carb snack.
- Talk to your doctor about an emergency kit.
Recognizing this early can prevent scary episodes.
5. Sleep Apnea: Breathing Pauses That Worsen Everything
Loud snoring, gasping for air, or daytime exhaustion? Sleep apnea and diabetes often go hand-in-hand.
Breathing interruptions reduce oxygen, stressing your body and making insulin resistance worse.
One truck driver saw his blood sugar control improve dramatically after starting CPAP therapy and losing some weight.
Helpful approaches:
- Sleep on your side.
- Manage weight gradually.
- Avoid alcohol in the evening.
Addressing this can lead to deeper rest and better overall health.
6. Nighttime Leg Cramps: Sudden, Painful Wake-Ups
Those intense calf or foot cramps that jolt you awake? They can stem from electrolyte shifts or circulation issues linked to high glucose.
Dehydration and mineral imbalances play a role too.
Relief ideas:
- Stay hydrated during the day.
- Stretch your calves before bed.
- Ensure good intake of magnesium and potassium-rich foods.
Simple changes often reduce these disruptions.
7. Intense Nighttime Thirst: Waking Up Parched
Constant dry mouth or thirst pulling you out of sleep? This pairs with frequent urination, as high blood sugar causes dehydration.
It’s your body’s way of signaling fluid loss.
What to do:
- Control daytime glucose for fewer overnight effects.
- Keep water bedside, but focus on root causes.
Common Misconceptions vs. Better Approaches
Here’s a quick comparison to clear up confusion:
| Sign | Common Misdiagnosis | Better Approach | Potential Benefit |
|---|---|---|---|
| Night Sweats | Menopause or anxiety | Check bedtime glucose | Fewer sweaty interruptions |
| Frequent Urination | Aging or prostate issues | Monitor daily blood sugar | Unbroken sleep |
| Restless Legs | Stress or poor mattress | Steady glucose + stretches | Calmer evenings |
| Leg Cramps | Dehydration alone | Electrolyte balance + hydration | Pain-free nights |
| Sleep Apnea | Just snoring | Weight management + side sleeping | Better oxygen and energy |
Your 8-Week Plan to Better Nights and Blood Sugar Control
Ready for actionable steps? Follow this phased approach:
- Weeks 1–2: Focus on Lows – Bedtime checks + small carb-protein snack if needed. Expect fewer wake-ups.
- Weeks 3–4: Calm Legs – Evening stretches, hydration, cut afternoon caffeine.
- Weeks 5–6: Breathing and Thirst – Side sleeping, limit evening fluids.
- Weeks 7–8: Overall Stability – Consistent monitoring, balanced meals.
Track progress weekly—you’ll likely notice more energy and deeper rest.
The Key Takeaway: Steady Blood Sugar Unlocks Restful Sleep
These nighttime signs all point to one core issue: the need for better daily blood sugar management through diet, monitoring, movement, and medication as prescribed.
Imagine a month from now—sleeping soundly, waking refreshed, with more vitality for what matters.
Starting tonight: Check your levels before bed. Small steps add up.
You’ve made it to the end—congrats on prioritizing your health!
Frequently Asked Questions
How many times is it normal to wake up at night to urinate?
Once is usually fine; two or more could indicate high blood sugar or other issues. Track it and discuss with your doctor.
Can these symptoms go away with lifestyle changes?
Many people see big improvements with consistent glucose control, better habits, and weight management if needed.
Should I wake my partner if I suspect low blood sugar at night?
Yes—train loved ones on signs and how to help with fast carbs or glucagon if prescribed.
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider if you experience these symptoms or have concerns about diabetes.
ADVERTISEMENT