ADVERTISEMENT
Many women quietly worry about changes in their body—like unexpected bleeding between periods, unusual discharge, or persistent pelvic discomfort that disrupts intimacy and daily routines. These shifts can spark anxiety, making you hesitate to speak up or seek help, especially when fears of something serious like cervical cancer creep in. You’re not alone in this—millions face similar concerns that affect confidence, relationships, and peace of mind. But here’s the good news: paying close attention to these signals and acting early can make all the difference. Keep reading to uncover the key facts that could empower you—and discover a simple shift in habits that many women wish they knew sooner.
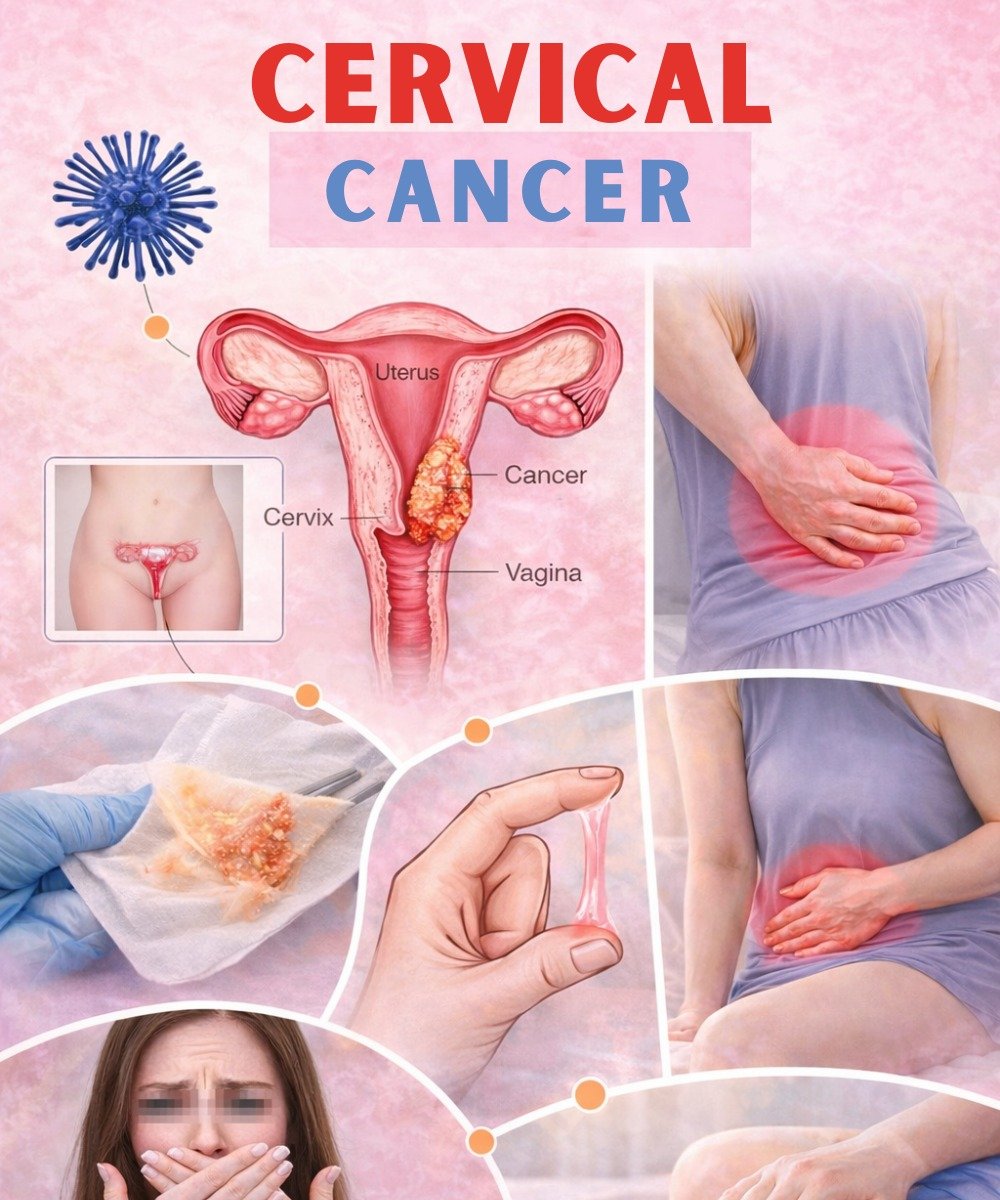
What Is Cervical Cancer and How Does It Develop?
Cervical cancer begins in the cells lining the cervix, the narrow passage connecting the uterus to the vagina.
Nearly all cases stem from long-term infection with high-risk strains of human papillomavirus (HPV), a very common virus passed through sexual contact.
Research from the World Health Organization (WHO) confirms that persistent HPV causes about 99% of cervical cancers.
The virus can linger silently for years, slowly causing cell changes that may turn precancerous if unchecked.
But that’s not the full story… Most HPV infections clear on their own thanks to a healthy immune system.
Factors like smoking, a weakened immune system, or multiple sexual partners can increase risks.
The truth is, cervical cancer is highly preventable—and understanding its roots is the first step toward protection.
Key Signs and Symptoms of Cervical Cancer
Early cervical cancer often flies under the radar with no obvious symptoms. That’s why so many cases go unnoticed until later stages.
When signs do appear, they can mimic other common issues, leading to delays.
If you’ve been brushing off persistent changes, know that early attention brings clarity and better outcomes.
Here’s what studies from the CDC and American Cancer Society highlight as potential warning signs:
- Abnormal vaginal bleeding: Spotting between periods, after sex, or even after menopause. This is one of the most common red flags as cancer advances.
- Unusual vaginal discharge: Watery, pink, bloody, or foul-smelling—changes that feel off and persistent.
- Pelvic pain or discomfort: Ongoing ache in the lower abdomen, hips, or back that doesn’t go away.
- Pain during intercourse: Discomfort or bleeding that strains intimacy and adds emotional worry.
Other possible indicators include unexplained fatigue, leg swelling, or unintended weight loss.
These aren’t unique to cervical cancer—conditions like infections or fibroids can cause them too.
But ignoring them? That could mean missing a chance for early intervention.
Sự thật là… many women experience relief just by talking to a doctor.
| Potential Symptom | Why It Matters | Common Emotional Impact |
|---|---|---|
| Abnormal bleeding | Often the first noticeable sign | Disrupts daily life and sparks fear |
| Unusual discharge | Signals possible cell changes | Affects hygiene and self-confidence |
| Pelvic or lower back pain | May indicate progression | Limits movement and enjoyment |
| Pain during intercourse | Points to cervical irritation | Strains relationships and intimacy |
Why Early Detection Is Crucial for Cervical Health
Precancerous changes rarely cause symptoms, allowing quiet progression over time.
Regular screening catches these early—when they’re easiest to address.
According to the CDC, screening has slashed cervical cancer deaths by over 50% in recent decades.
If anxiety about symptoms has delayed your check-ups, you’re not alone.
But here’s the empowering part: the latest 2025 guidelines from the American Cancer Society make screening more accessible than ever.
They recommend starting at age 25 with primary HPV testing every 5 years up to age 65 (preferred method).
Clinician-collected samples are ideal, but self-collection options for HPV testing are now acceptable— a game-changer for convenience.
Alternatives include Pap tests every 3 years or co-testing.
Research shows these approaches detect issues early, often before symptoms start.
The most interesting thing? Consistent screening means many precancers never become cancer.
Practical Steps to Prevent Cervical Cancer
Prevention starts with smart, doable habits backed by science.
If concerns about signs have motivated you, these steps can reduce risks significantly.
- Get vaccinated against HPV: The vaccine protects against high-risk strains causing most cases. Ideally starting at ages 9-12, it’s recommended through age 26—and shared decision-making for ages 27-45 if not previously vaccinated (per CDC).
- Practice safer sex: Consistent condom use and fewer partners lower HPV transmission.
- Quit smoking: It impairs your body’s ability to fight HPV.
- Stay up-to-date on screenings: Follow guidelines tailored to your age and history.
Here’s a simple action plan you can start today:
- Schedule a chat with your doctor about your HPV vaccination status.
- Book your next screening if it’s due—ask about self-collection options.
- Track any persistent symptoms in a journal to discuss openly.
- Explore quit-smoking resources if needed (like apps or support lines).
These habits not only target cervical health but boost overall well-being.
And remember… vaccination plus screening is the powerful duo driving down rates.
Take Control of Your Cervical Health Today
Recognizing potential signs of cervical cancer doesn’t have to mean fear—it means empowerment.
With nearly all cases linked to preventable HPV, early detection through screening and vaccination offers real hope.
Many women who’ve acted early share stories of relief and positive outcomes.
Talk to your healthcare provider about any worries, get screened regularly, and consider vaccination if eligible.
Your body deserves this attention—and the peace of mind that follows is priceless.
Frequently Asked Questions
When should I start cervical cancer screening?
The American Cancer Society recommends beginning at age 25 with primary HPV testing every 5 years (or alternatives like Pap tests). Consult your doctor for personalized timing based on risks.
Do these symptoms always indicate cervical cancer?
No—many have benign causes like infections or hormonal shifts. Persistent ones, however, warrant a professional check to rule out concerns.
Can the HPV vaccine help if I’m already sexually active?
Yes, it can still protect against HPV strains you haven’t encountered. Benefits are greatest before exposure, but it’s worth discussing with your provider up to age 45.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for personalized guidance, especially if experiencing symptoms or due for screening. Early professional care is key to health.
ADVERTISEMENT